With the United Nations High Level meeting just over the horizon, the tuberculosis (TB) community is poised and ready to amplify the voices of people affected by TB around the world at this global forum, and demand the global attention and resources needed to beat this devastating yet curable disease. Doctors Without Borders/Médecins Sans Frontières (MSF) is one of the main non-governmental providers of TB care worldwide, especially for people with drug-resistant TB, and helps lead global efforts to make newer, more effective treatments affordable and available to those who need them.
In this blog, Christophe Perrin, the MSF Access Campaign‘s TB advocacy pharmacist, talks to us about the new energy around TB today that builds on MSF’s long-term engagement to secure affordable access to improved TB medicines for people in MSF’s care and beyond. In particular, he focuses on the long battle to secure access to the key TB drug, bedaquiline which has become the cornerstone of all the recommended treatments for people with drug-resistant TB (DR-TB) from the World Health Organization.
TB hasn’t grabbed the headlines much in the past but now there’s a lot more interest around TB—and specifically around the access to the key TB drug, bedaquiline?
Yes! We have indeed seen a flurry of announcements around the prices for bedaquiline over the last couple of months from Johnson & Johnson (J&J) who make bedaquiline, as well as from generic medicines producers in India. It’s a very complex story but taken all together it does mean that many more people will now get access to bedaquiline. That said, there’s still a mountain to climb and our key target remains J&J whose patents are blocking full access to this lifesaving drug.
Why is bedaquiline so important?
Bedaquiline has been an absolute gamechanger for our progress in treating and curing people with drug-resistant TB (DR-TB). When the first positive pre-clinical trial results for the drug were announced in 2009, we were very excited. TB doctors everywhere were only too aware about the lack of new drugs developed for TB for decades.
As a result, we and other physicians had to treat people with DR-TB with awful old toxic drugs, administered through painful daily injections, which usually failed to cure them, and in the process made them deaf or triggered psychosis or generated other terrible side effects.
So, when further trials continued to return positive results, we were determined to get hold of the medicine for people in our care. At this point in the development process, the drug wasn’t authorised for use yet, so we had to come up with a plan: a request for ‘Compassionate Use’ (CU) access to J&J offered the best possibility to getting this drug to people who needed it.
Is this a moment of hope for the TB community?
Yes, we opened negotiations with J&J who were initially reluctant, but after sharing evidence on how the same CU process had already been used to save the lives of people with HIV and cancer, they finally agreed. Other physicians, outside MSF projects, were also able to access the drug through CU and saw how people with TB—seemingly at death’s door—recovered once they were treated with bedaquiline combined with other approved medicines. It was indeed a moment of great hope for the TB community.

But J&J had other plans for bedaquiline once it became an authorised medicine?
Yes, as soon as it was authorized, J&J set out a pricing strategy that put the medicine out of reach of people in lower- and middle-income countries. Given that bedaquiline is just one of a combination of drugs required to treat people with DR-TB, the full treatment price per person ranged between $2000-$5000 USD—a price that no low-income country anywhere could afford. The TB community called out these prices publicly and, under pressure, J&J agreed on a time-limited donation program.
Did the donation solve the problem of access?
No. You can’t rely on donations as a permanent solution for access , as we saw five years later when J&J’s donation program ended. But at least during this period, the program helped more countries get hold of the medicine, save lives, and include bedaquiline in their national TB treatment guidelines.
Why did you launch a public campaign against J&J?
Once the donation program came to an end in 2019, J&J promptly announced once-again excessive prices for bedaquiline. Once more, people living with DR-TB were faced with an unsurmountable price barrier to getting lifesaving treatment. That’s when MSF mobilized and went public with the Dollar a Day campaign, demanding that J&J reduce the price of medicine to a dollar a day. Our civil society and treatment provider partners were alongside us in this cause.

What kind of arguments did you use to back up the campaign?
We were able to be very data driven, for instance by showing how, based on an analysis of the costs of production and including an adequate profit margin, J&J could be selling bedaquiline at least four times less than the price they were charging.
We also shared some other research too that calculated public investments made by the United States in the development of bedaquiline was up to five times the investment made by the corporation. So, J&J’s argument that they had to charge high prices to cover the development costs of bedaquiline and also for the development of future drugs in the pipeline were revealed as a sham. J&J eventually conceded by offering a 30 percent price reduction in 2020. So, it was a successful campaign, though the price still remained far too high to meet the needs of all people who needed bedaquiline in lower- and middle-income countries.
Tell us more about how generic production helps bridge the access gap.
When MSF and other care providers first faced the barriers to treatment for people living with HIV, created by the high price of antiretroviral drugs, we decided to pursue quality-assured generic production as a solution. Generic medicines producers drive drug prices down through the market competition they create. We and other civil society groups knew the same approach would bring down prices for bedaquiline, once the 20-year patent on the drug ran out.
Now J&J's "primary" patent for bedaquiline was due to run out on July 18th, 2023. Exploratory discussions with generic manufacturers in India revealed at least two key drug manufacturers interested in producing generic bedaquiline. Things were looking quite hopeful.
But J&J had another trick up their sleeve. Back in 2007, they had filed for "secondary" patents on bedaquiline. Unfortunately, many countries—including those with a high burden of TB—granted these secondary patents to J&J, with the result that J&J's monopoly on the medicine was extended in those countries from 2023— when the ‘primary’ patent expired—until at least 2027. That means countries face at least four more years of high prices, created by a company monopoly that has already made significant profits.
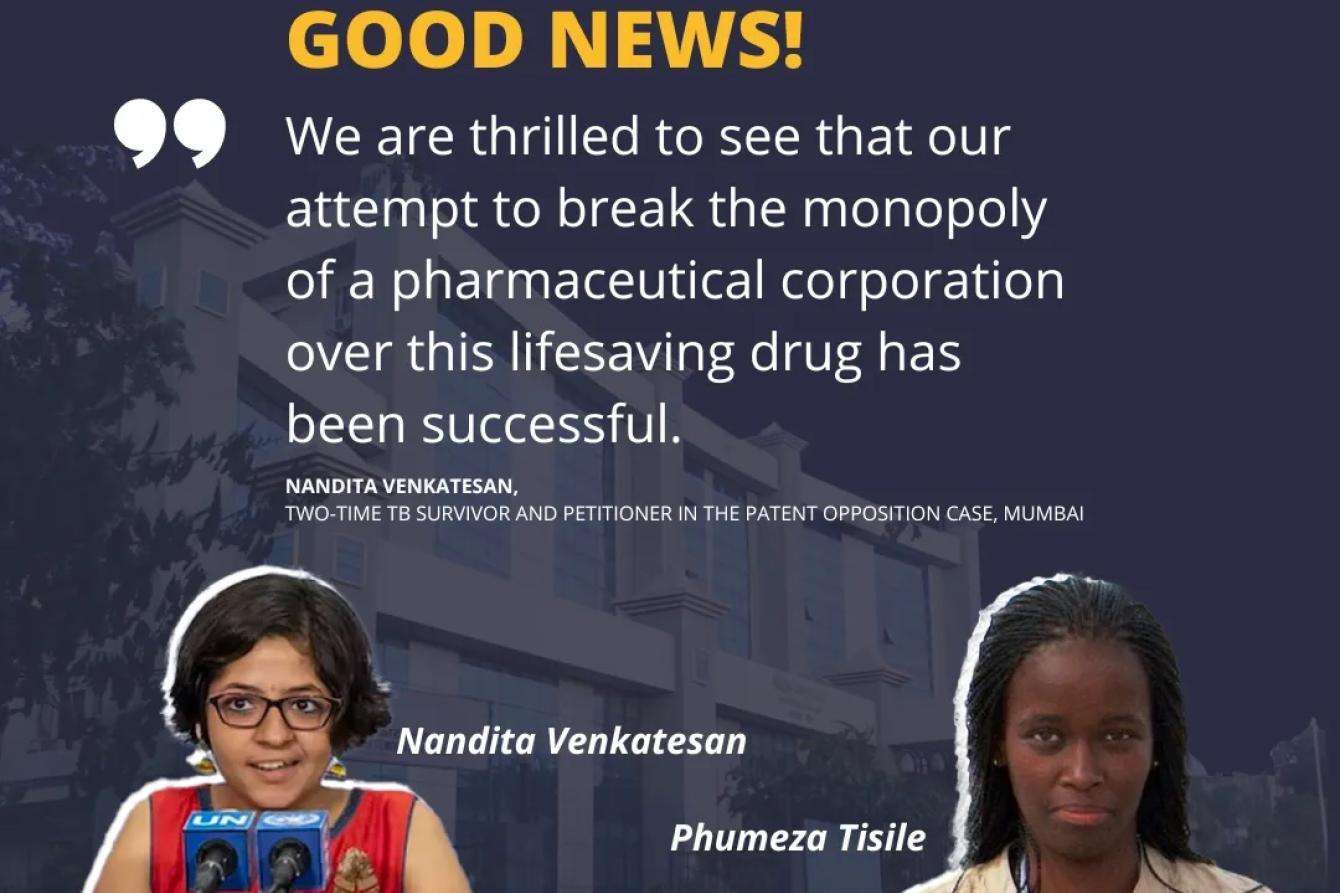
There was one shaft of light—back in 2019, members of the Access Campaign’s legal team in India had already spotted the amended secondary patent claims submitted by J&J in India, which were a verbatim copy of its earlier patent application on an HIV drug. Together with the Lawyers Collective, they were thus able to lend their legal support to two quite extraordinary DR-TB survivors-turned-activists, Nandita Venkatesan from India and Phumeza Tisile from South Africa, who teamed up to challenge the validity of the secondary patent through the patent office in India. Earlier this year, the Court struck down the secondary patent in India opening the way for generic manufacturers in India—at least—to move ahead with producing generic bedaquiline.
But to be clear, in countries where the secondary patents for bedaquiline are still in place, the affordable generics from India cannot be sold?
That’s right. That’s why the focus of our latest advocacy strategy has been to publicly call on J&J not to enforce its secondary patents in any country with a high burden of TB. In fact, J&J managed to pull off quite a publicity stunt around this whole secondary patents challenge despite the corporation’s patents still blocking access to generic bedaquiline.
J&J made a deal in July with the Global Drug Facility (GDF), an international drug pooled procurement organisation, to allow the supply of generic versions of bedaquiline to a list of low- and middle-income countries, including to some countries where J&J still holds patents on bedaquiline. But this deal is only available to those countries on the list who buy from the GDF directly.
As such, a high-TB-burden country like South Africa which has national procurement rules that prevent it from procuring through a pooled procurement organization like GDF, will not benefit from the deal. Other countries with a high burden of DR-TB are also excluded from the deal, including 9 countries in the Eastern Europe and Central Asia (EECA) region, which have some of the world’s highest burden of drug-resistant TB (Armenia, Azerbaijan, Belarus, Kazakhstan, Kyrgyzstan, Moldova, Tajikistan, Turkmenistan, and Ukraine).
In late August this year, J&J responded to generic manufacturers entering the market by lowering the price at which bedaquiline can be procured through GDF by 55 percent. This is a positive move, but this lower price is expected to soon be eclipsed by even lower generic prices from Indian manufacturers. Therefore, it is a short-term solution, as eventual access to the lowest-price generic will be blocked in the future for countries excluded from the deal due to J&J’s patent barriers.
It sounds very complicated!
It is! And that lack of clarity does nothing to help people with TB. The take-away from all this is that J&J’s aggressive strategy of holding on to its patents, for a medicine developed largely with public funds, is standing in the way of treatment for many people living with DR-TB around the world.
What’s next?
Alongside other treatment providers and civil society partners in this effort, we will carry on calling on J&J not to enforce secondary patents on bedaquiline. And this will be one strand of our work in standing alongside people with TB at the global forum of the United Nations High-Level Meeting in New York this month. Together, MSF and its allies will raise their voices at this meeting where the global spotlight will be on TB to ensure that beating this ancient, yet curable disease is irreversibly printed on the global agenda.



